Therapy
The general goal of therapeutic measures for craniosynostosis is to eliminate, mitigate or prevent as many of the negative consequences of synostosis as possible, thereby creating optimal conditions for the child's development. Depending on the form and characteristics of the synostosis, aesthetic aspects or reasons such as lowering of increased pressure in the head or protection of the eyes by enlarging the eye socket are in the foreground.
Depending on the form of synostosis, there are two surgical principles, which are performed in joint work by pediatric neurosurgery and oral and maxillofacial surgery.
Passive remodeling
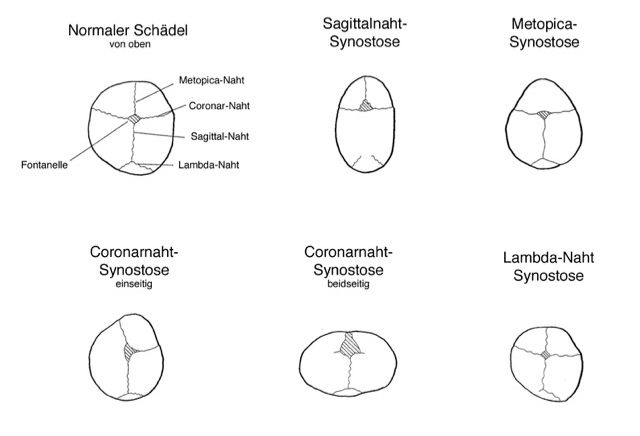
In passive remodeling, as used for sagittal suture synostosis, for example, the correspondingly ossified cranial suture and the adjacent bones of the cranial calvaria are removed. Within a few months, the bone is remodeled by the body (called reossification) and the skull is remodeled in the interval in between according to the shaping force of the growing brain. This operation should be performed between the 5th-6th month of life, because at this time of maximum brain growth the internal pressure in the head is highest and the reossification also occurs without problems. Surgery at an earlier time, e.g. at 3 months of age, requires additional treatment with a helmet to support the reshaping. This early endoscopically assisted therapy offers advantages especially in metopica and coronary suture synostoses, as a later, reshaping and major surgery can often be avoided.
Active remodeling
Active remodeling is used, for example, in frontal suture/metopicasynostosis or isolated coronal suture synostosis at the age of 10-12 months. In this case, the skull bone in the area of the forehead and the roof of the orbit, including the ossified suture, is removed, divided into suitable segments, actively remodeled and then reassembled in the desired shape and fixed to the base of the skull. This improves the deformity in the area of the forehead and ocular skeleton and, in the case of syndromal craniosynostoses, also creates space in the head.
In some synostoses, a backward extension of the skull is also applied.
The most important risk of these operations is relevant blood loss, which is mainly due to the large wound area. In this case, the administration of blood reserves and clotting factors is often necessary despite all blood-saving surgical techniques and measures taken during the operation as a rule. After the operation, the children spend one night in our pediatric intensive care unit to ensure optimal care and monitoring of blood values. The total inpatient stay is between 4-7 days, depending on the type of surgery and the age of the child.
The probability of a craniosynostosis recurring after a successful operation, i.e. the space for the brain becoming too small so that a second operation is necessary, is a maximum of 10% for isolated synostoses and at least 60% for syndromes with many affected sutures.
Follow-up
After surgery, children are followed up regularly for years in our craniofacial consultation by a team of pediatric neurosurgeons, oral and maxillofacial surgeons, and neuropediatricians to detect any recurrences early.